More than 100 peer-reviewed science and medical journal articles demonstrate the benefits of BrainHQ brain fitness technology. Currently, 60+ of these articles address benefits to healthy aging adults, while 40+ articles address the impact on patients with health conditions (eg, depression, MCI, stroke, brain injury, chemobrain, schizophrenia). This report summarizes improvements to people across a wide spectrum, with a particular focus on what has been shown in research on clinical conditions. Citations appear in brackets, below, and tie to the journal articles listed at the end.
This report builds on a prior report on the impact of BrainHQ exercises and assessments on normal aging, which can be found in the healthy aging section. That prior report showed that BrainHQ assessments and exercises measure and improve basic cognitive function, and that training with the exercises generalizes to improve key standard measures of cognitive function (including, speed and accuracy of processing, attention, memory, executive function and every day cognition), as well as various standard measures of quality of life (including functional independence, mood and control, health outcomes and mobility). The impact of the BrainHQ brain exercises on healthy adults appears to be as broad and far-reaching as the impact of physical exercise, except the effects (i) require less time, (ii) diminish more slowly and (iii) impact the cognitive realm more deeply.
Researchers have now extended the findings of generalized improvements in standard measures of cognitive function and quality of life from healthy adults to people grappling with clinical conditions that include cognitive deficits. For simplicity, this report groups clinical conditions into three areas: mental illness, brain injury and neurodegenerative disorders. To some extent, these are artificial groupings that are both too broad and too narrow -- since each individual cognitive disorder within these groups has its own particular set of symptoms and since many individual symptoms are commonly found across disorders in all of these groups.
Put another way, it is worth noting that while people may find they have cognitive deficits from very different causes (eg, advanced aging, chronic schizophrenia, head injury), the symptoms are not all that different, and many of the same tools and strategies can be employed to address them. BrainHQ from BrainHQ is an online resource with dozens of cloud-based exercises designed to provide a broad array of tools to address many different cognitive deficits.
Except as otherwise noted, all studies cited in this report were (i) of BrainHQ assessments and exercises, (ii) examined in blinded, randomized controlled trials, (iii) had results that were statistically significant, (iv) have been published in peer-reviewed journals, and (v) were conducted by independent researchers.
This report is not recommending BrainHQ exercises for treatment of any disease or disorder; rather, it is reporting on the current state of the science in these areas for the education of healthcare and other professionals interested in developments in these areas.
Mental Illness
Schizophrenia. There are now numerous studies and reviews examining the impact of BrainHQ exercises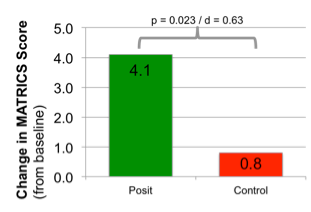 in people with schizophrenia. [citations 1,2,3,4,5,6,7,8,9,10,11,12,13, 14,15,16,17,18,19] Schizophrenia is often described in terms of its “positive” and “negative” symptoms. Positive symptoms, such as delusions, are often effectively treated with anti-psychotic pharmaceuticals. Negative symptoms, which typically include deficits in basic cognitive functions, are largely untreated, and are often what make it difficult for a person with schizophrenia to hold a job and live independently. Government and big pharma have agreed on a battery of cognitive measures, called the MATRICS Battery, to be used in examining the effectiveness of cognitive-enhancing drugs designed to treat schizophrenia. To date, no study has shown any drug yields significant gains on the MATRICS Battery. A number of studies of BrainHQ exercises have shown it improves cognition sufficiently to drive significant gains on MATRICS Battery [3,4,5,6,7,16,18]. A BrainHQ exercise regimen is now in an NIMH-funded pivotal trial for submission to the FDA. These gains are not just in the task trained, but generalize to standard measures of cognition, including significant gains in standard measures of attention, memory, speed of processing, executive function, and social cognition, as well as improvements in both auditory and visual-spatial processing. Studies in these areas have typically involved a large amount of training over many months, often with computer games used as an active control. Gains are highly correlated with progress in the exercises. [3] Researchers have found that the gains from training
in people with schizophrenia. [citations 1,2,3,4,5,6,7,8,9,10,11,12,13, 14,15,16,17,18,19] Schizophrenia is often described in terms of its “positive” and “negative” symptoms. Positive symptoms, such as delusions, are often effectively treated with anti-psychotic pharmaceuticals. Negative symptoms, which typically include deficits in basic cognitive functions, are largely untreated, and are often what make it difficult for a person with schizophrenia to hold a job and live independently. Government and big pharma have agreed on a battery of cognitive measures, called the MATRICS Battery, to be used in examining the effectiveness of cognitive-enhancing drugs designed to treat schizophrenia. To date, no study has shown any drug yields significant gains on the MATRICS Battery. A number of studies of BrainHQ exercises have shown it improves cognition sufficiently to drive significant gains on MATRICS Battery [3,4,5,6,7,16,18]. A BrainHQ exercise regimen is now in an NIMH-funded pivotal trial for submission to the FDA. These gains are not just in the task trained, but generalize to standard measures of cognition, including significant gains in standard measures of attention, memory, speed of processing, executive function, and social cognition, as well as improvements in both auditory and visual-spatial processing. Studies in these areas have typically involved a large amount of training over many months, often with computer games used as an active control. Gains are highly correlated with progress in the exercises. [3] Researchers have found that the gains from training 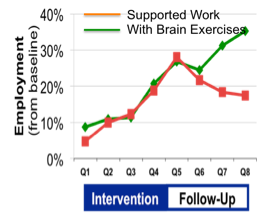 persist for six months after training ends, but do wane over time without further training [7]. Researchers have found that training drives measurable changes in the brain itself. Many such changes were observable through imaging, including increased activity in the amygdala [11,14] putamen and prefrontal cortex (associated with improved emotion perception and social cognition) [11], as well as increased time-locked gamma band response and non-time-locked alpha band desynchronization (associated with improved verbal memory) [9] and increased mPFC activity (associated with improved social functioning) [10]. In a 72-person randomized controlled trial (with a third arm matched set of healthy controls), researchers also found significant gains in Brain Derived Neurotrophic Factor (a growth factor associated with neural health and typically at low levels in people with schizophrenia) among patients who did BrainHQ exercises, as compared to the computer game control. [6] Perhaps, most importantly, researchers have found that training generalizes to increased ability to hold a job [1,2,19], and that ability continues for at least 2 years after training ends, though the effects wane without further training [15].
persist for six months after training ends, but do wane over time without further training [7]. Researchers have found that training drives measurable changes in the brain itself. Many such changes were observable through imaging, including increased activity in the amygdala [11,14] putamen and prefrontal cortex (associated with improved emotion perception and social cognition) [11], as well as increased time-locked gamma band response and non-time-locked alpha band desynchronization (associated with improved verbal memory) [9] and increased mPFC activity (associated with improved social functioning) [10]. In a 72-person randomized controlled trial (with a third arm matched set of healthy controls), researchers also found significant gains in Brain Derived Neurotrophic Factor (a growth factor associated with neural health and typically at low levels in people with schizophrenia) among patients who did BrainHQ exercises, as compared to the computer game control. [6] Perhaps, most importantly, researchers have found that training generalizes to increased ability to hold a job [1,2,19], and that ability continues for at least 2 years after training ends, though the effects wane without further training [15].
Depressive Symptoms and Mood.. In a study of 1,606 older adults with no depression at baseline, 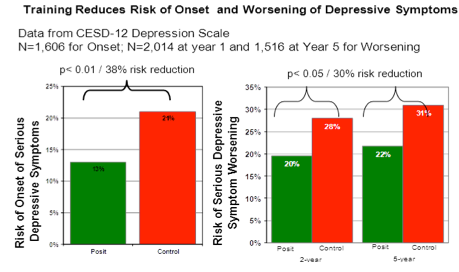 researchers found that those who trained with a BrainHQ exercise (for just 10 hours) were 38% less likely a year later to experience onset of clinically significant depressive symptoms, as compared to the control group. [20] Similarly, looking at 1,516 subjects over a five-year period, they found those who did the exercises were 30% less likely to have a clinically significant worsening of depressive symptoms on the subsequent test date (at years 2 and 5). [21] In addition, using the locus of control measure, in a study of 1,534 older adults, researchers found that those who did BrainHQ training had much greater feelings of control over their lives and more confidence in their everyday activities, than those in the control group [22].
researchers found that those who trained with a BrainHQ exercise (for just 10 hours) were 38% less likely a year later to experience onset of clinically significant depressive symptoms, as compared to the control group. [20] Similarly, looking at 1,516 subjects over a five-year period, they found those who did the exercises were 30% less likely to have a clinically significant worsening of depressive symptoms on the subsequent test date (at years 2 and 5). [21] In addition, using the locus of control measure, in a study of 1,534 older adults, researchers found that those who did BrainHQ training had much greater feelings of control over their lives and more confidence in their everyday activities, than those in the control group [22].
Bi-polar. A recent first small single-arm pilot among veterans with bi-polar, published as a poster, found participants improved at the exercises and on standard measures of attention and memory [P1].
Brain Injury
Traumatic Brain Injury (TBI). A BrainHQ assessment, UFOV®, has been shown effective in number of studies for assessing the safe-driving ability of people with TBI [23,24,25], and BrainHQ exercises have repeatedly been shown to improve performance at that assessment. In a single-arm feasibility study, researchers at Mt Sinai Hospital found that training people with mild to severe TBI to use BrainHQ exercises from home was feasible. They also found gains on the standard cognitive measures used by the military, including ANAM-4, CFQ and FrSBe, indicating improvements in attention, memory, speed and executive function, as well as improvement in self-reported failures in perception, memory, and motor control and in executive dysfunction, apathy and disinhibition. [26] The Mt Sinai team had previously run a similar study, but with training conducted in an in-patient setting, which was published as a poster and had similar results [P2]. In a small 2014 randomized controlled trial published as a poster, researchers found people with traumatic brain injury who used the BrainHQ auditory training had significant improvement on measures of auditory and visual processing speed (d = .89 and .56, respectively), set-shifting (d = .76), following verbal directions (d = .47), and non-verbal reasoning correct responses and reaction time (d = .44 and .50, respectively). [P3]
Cardiobrain. Recognizing that many patients with heart failure have cognitive deficits as a result of the related brain injury from a weak heart, researchers in the MEMOIR Study investigated whether BrainHQ exercises would deliver benefits. In this 40 person randomized controlled trial, the intervention group trained for 40 hours on brain exercises. They showed significant gains in standard measures of memory, processing speed and functional independence, as compared to the active control, which engaged in health education activities. [27] In addition, researchers found a trend (p=.24) indicating the intervention group consumed fewer health resources and had half the healthcare costs of the control group. [28] In another randomized controlled trial of 54 older adults with heart failure, researchers found those who trained with a BrainHQ exercise performed significantly better at a measure of speed of processing (associated with better functional independence) than the control group. [29] Chemobrain. An estimated 17% of cancer patients have persistent cognitive issues after chemotherapy (“chemobrain”). [30] In an 82- person randomized controlled trial, researchers tested BrainHQ visual training against a memory course and a no contact control. Researchers found the BrainHQ exercises resulted in immediate and durable improvements in objective measures of processing speed and verbal memory, as well as on standard measures of perceived cognitive functioning, symptom distress (anxiety, mood disturbance and fatigue) and quality of life. While the memory course also yielded significant results, the BrainHQ exercises yielded larger, more immediate and more durable improvements in objective measures of processing speed and verbal memory. [30] The study confirmed findings in a smaller pilot, published as a poster, showing statistically significant improvements in health-related quality of life, stress levels, and self-reported cognitive function, following training, as compared to a no-contact control group. [P4] Stroke. Studies have shown a BrainHQ assessment is effective in determining automotive driving risk after stroke. [31,32,33] In a 24-person trial among patients recovering from stroke, with moderate to severe neglect, those using BrainHQ visual training demonstrated significant improvement in several untrained measures of spatial and non-spatial visual attention, and failed to demonstrate a lateralized attention deficit, as compared to the wait group control. The intervention involved just a total of 5 hours of brain exercise spread over 9 days, and also showed significant improvements on standard measures of visual search, midpoint estimation and working memory against the control. [34] In a subsequent study, a similar continuous task auditory training also demonstrated significant improvement in several untrained measures of spatial and non-spatial visual attention, and failed to demonstrate a lateralized attention deficit, as compared to the wait group control. [35] In a 52-person trial, researchers found a substantial reduction in visual attention after stroke, which could be significantly improved by BrainHQ training. [36] HIV. Patients with chronic HIV infection experience a pre-mature aging of the brain known as HIV-Acquired Neurological Disorder (HAND). [37] In a 46-person randomized control trial among people with HIV, those training on BrainHQ exercises, as compared to the no contact control, showed significant improvements in three cognitive measures and one functional measure: speed of processing (UFOV), psychomotor (finger tapping), executive function (Wisconsin card sorting) and functional independence (TIADLs). They also improved in self-report cognitive measures at exit. [37] In a follow-up analysis, researchers found that UFOV and TIADL scores at baseline were highly correlated (underscoring that speed of processing and attention are instrumental to both assessments) and that those with low scores demonstrated significantly more training gains. [38]
Neurodegenerative Disorders
Pre-Dementia (MCI). In a small fMRI imaging trial of people with Mild Cognitive Impairment, or MCI, (a 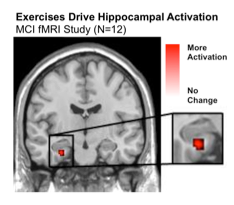 pre-dementia condition with significant memory impairment), those who trained with auditory exercises improved significantly in verbal memory and showed significant increases in left hippocampal activation relative to the computer game control group. [39] In a related pilot, people with MCI who trained with BrainHQ exercises showed evidence for improvements in immediate and delayed measures of verbal memory. With no further training, effects waned, but between group differences persisted for a year. [40]
pre-dementia condition with significant memory impairment), those who trained with auditory exercises improved significantly in verbal memory and showed significant increases in left hippocampal activation relative to the computer game control group. [39] In a related pilot, people with MCI who trained with BrainHQ exercises showed evidence for improvements in immediate and delayed measures of verbal memory. With no further training, effects waned, but between group differences persisted for a year. [40]
Parkinson. Patients with mild to moderate Parkinson Disease who used the BrainHQ remediation experienced significantly greater improvements on UFOV performance than the no contact control group. [41] UFOV performance has been correlated to driving performance and other measures related to aging. [41] In a driving study of 19 people with Parkinson Disease, compared to 104 healthy controls, researchers found that, when compared to neuropsychological tests of vision and cognition, the BrainHQ test showed the strongest correlations (r > .75) with measures of failing a standard road test and with number of driving errors. [42]
Multiple Sclerosis. A recent study compared 50 people with Multiple Sclerosis (MS) and 50 healthy controls using a BrainHQ assessment and the ASDE driver test. Researchers found people with MS performed worse in attention, information processing, working memory and visuo-motor coordination tasks. [43] Two prior studies of people with MS showed a significant correlation between poor scores on the BrainHQ assessment and elevated crash risk and incidence. [44,45] A recently published poster of a 10-person single-arm study of BrainHQ training, by adults with MS, found: (1) a high rate of exercise program compliance and (2) a positive treatment signal with improvement on exercises, participant ratings, and standardized cognitive measures. [P5]
How It Works
These results indicate that there is something special about the BrainHQ exercises. There are more than 100 issued patents with more than 1,000 patent claims underlying the technology in these exercises. Cognitive scientists from around the world have brought their best ideas to this work and look to make each part of every exercise as powerful as possible, so explaining how they work in a comprehensive manner is daunting.
Simply put, however, the exercises are based on a handful of powerful ideas. Unlike previous cognitive training, they do not try to fix a problem by practicing it – eg, they don’t improve memory by practicing memory. Instead, the exercises start with elemental cognitive function by first improving the speed and accuracy of your sensory perceptions. This becomes the foundation for improved attention. Improved attention is the building block of working memory, and working memory is the building block of pretty much everything else – immediate memory, delayed memory, episodic memory, executive function, reasoning, speech and language, visual-spatial skills, etc. No one has taken this complete bottom up approach to cognitive training before.
In addition, our scientists are experts in brain plasticity, the ability of the brain to re-wire and change. Each exercise draws on what experts have learned in recent years about driving change in the brain. Training needs to be focused on improving speed to meet varying real world conditions; it needs to intensively and progressively improve accuracy; it needs to be adapting continuously and minutely (eg by thousandths of a second) to each person’s performance and ability (based on algorithms that review all prior exercises results); it needs to be designed so the task gradually generalizes to real world experience; it needs to be engaging in a manner that naturally stimulates neurotransmitters (chemicals in the brain that enhance attention, learning and mood) and that brings you back to do the exercises again and again.
What’s Next?
BrainHQ maintains an active research and development effort, with new exercises, assessments and studies. Currently, there are more than 100 published journal articles on the benefits of these exercises and assessments, with dozens of other studies underway or completed and on their way to publication. You can stay up to speed by signing up for our newsletter.
Citations:
- Greig TC, Zito W et al. Improved Cognitive Function in Schizophrenia After One Year of Cognitive Training and Vocational Services. Schizophr Res 2007 Nov;96(1-3):156-61.
- Bell MD, Zito W et al. Neurocognitive enhancement therapy with vocational services: work outcomes at two-year follow-up. Schizophr Res 2008;105(1-3):18–29.
- Adcock RA, Dale C et al. When top-down meets bottom-up: auditory training enhances verbal memory in schizophrenia. Schizophr Bull 2009 Nov;35(6):1132-41.
- Fisher M, Holland C et al. Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. Am J Psychiatry 2009 Jul;166(7):805-11.
- Vinogradov S, Fisher M et al. The cognitive cost of anticholinergic burden: Decreased response to cognitive training in schizophrenia. Am J Psychiatry 2009;166(9):1055.
- Vinogradov S, Fisher M et al. Is serum brain-derived neurotrophic factor a biomarker for cognitive enhancement in schizophrenia? Biological Psychiatry 2009;66(6):549–53.
- Fisher M, Holland C et al. Neuroplasticity-based cognitive training in schizophrenia: an interim report on the effects 6 months later. Schizophr Bull 2010 Jul;36(4):869-879.
- Fisher M, Loewy R et al. Cognitive interventions targeting brain plasticity in the prodromal and early phases of schizophrenia. Annual review of clinical psychology. 2013;9:435–63.
- Popov T, Rockstroh B et al. Adjusting Brain Dynamics in Schizophrenia by Means of Perceptual and Cognitive Training. PloS one. 2012;7(7):e39051.
- Subramaniam K, Luks TL et al. Computerized cognitive training restores neural activity within the reality monitoring network in schizophrenia. Neuron. 2012;73(4):842–53.
- Hooker CI, Bruce L et al. Neural activity during emotion recognition after combined cognitive plus social cognitive training in schizophrenia. Schizophr Res 2012 Aug;139(1-3):53-9.
- Keefe RS, Vinogradov S et al. Feasibility and pilot efficacy results from the multisite cognitive remediation in the schizophrenia trials network (CRSTN) randomized controlled trial. J Clin Psychiatry. 2012 Aug;73(7):1016–22.
- Panizzutti R, Hamilton SP, Vinogradov S. Genetic correlate of cognitive training response in schizophrenia. Neuropharmacology. 2013; 64:264–7
- Hooker CI, Bruce L et al.. The influence of combined cognitive plus social-cognitive training on amygdala response during face emotion recognition in schizophrenia. Psychiatry Res. 2013 Aug 30;213(2):99-107.
- Bell MD, Choi KH, Dyer C, Wexler BE. Benefits of Cognitive Remediation and Supported Employment for Schizophrenia Patients with Poor Community Functioning. Psychiatr Serv. 2014 Apr 1;65(4):469-75.
- Fisher M, Loewy R et al. Neuroplasticity-Based Auditory Training Via Laptop Computer Improves Cognition in Young Individuals With Recent Onset Schizophrenia. Schizophr Bull. 2014 Jan 20;sbt232.
- Nahum M, Fisher M et al. A novel, online social cognitive training program for young adults with schizophrenia: A pilot study. Schizophrenia Research: Cognition. 2014;1(1):e11–19.
- Sacks S, Fisher M et al. Combining computerized social cognitive training with neuroplasticity-based auditory training in schizophrenia. Clinical schizophrenia & related psychoses. 2013;7(2):78–86A
- Subramaniam K, Luks TL et al. Intensive cognitive training in schizophrenia enhances working memory and associated prefrontal cortical efficiency in a manner that drives long-term functional gains. NeuroImage. 2014 Oct 1;99:281-92.
- Wolinsky FD, Mahncke HW et al (2009). The ACTIVE cognitive training interventions and the onset of and recovery from suspected clinical depression. J Gerontol B Psychol Sci Soc Sci, 64B(5), 577-85.
- Wolinsky FD, Vander Weg MW et al (2009). The effect of speed-of-processing training on depressive symptoms in ACTIVE. J Gerontol A Biol Sci Med Sci, 64A(4), 468-72.
- Wolinsky FD,Vander Weg MW et al (2009). Does Cognitive Training Improve Internal Locus of Control Among Older Adults? J. Gerontol B Psychol Sci Soc Sci, 2010 Sep;65(5):591-8. doi: 10.1093/geronb/gbp117.
- Fiske GD, Novack T et al. Useful field of view after traumatic brain injury. J Head Trauma Rehabil 2002 Feb;17(1):16-25.
- Novack TA, Banos JH et al. UFOV performance and driving ability following traumatic brain injury. Brain Inj. 2006 May;20(5):455-61
- Calvanio R, Williams R et al. Acquired brain injury, visual attention, and the useful field of view test: A pilot study. Arch Phys Med Rehabil. 2004 Mar;85(3):474-8.
- Lebowitz MS, Dams-O’Connor K, Cantor JB. Feasibility of computerized brain plasticity-based cognitive training after traumatic brain injury. JRRD 2012:49 1547-1556
- Pressler J, Therrien B et al. Nurse-Enhanced Memory Intervention in Heart Failure: The MEMOIR Study. Journal of Cardiac Failure. 2011; 17(10)
- Pressler SJ, Martineau A et al. Healthcare resource use among heart failure patients in a randomized pilot study of a cognitive training intervention. Heart Lung. 2013 Sep-Oct; 42(5) 332-8.
- Ellis ML, Edwards JD et al. Effects of Cognitive Speed of Processing Training Among Older Adults With Heart Failure. J Aging Health June 2014 vol. 26 no. 4 600-615 doi: 10.1177/0898264314525666
- Von Ah D, Carpenter JS et al. Advanced cognitive training for breast cancer survivors: a randomized controlled trial. Breast Cancer Res Treat. 2012 Oct;135(3):799-809.
- Mazer BL, Sofer S et al. Effectiveness of a visual attention retraining program on the driving performance of clients with stroke. Arch Phys Med Rehabil. 2003 Apr;84(4):541-50
- Fisk GD, Mennemeir M. Common neuropsychological deficits associated with stroke survivors' impaired performance on a useful field of view test. Percept Mot Skills. 2006 Apr;102(2):387-94.
- George S, Crotty M. Establishing criterion validity of the Useful Field of View assessment and Stroke Drivers' Screening Assessment: comparison to the result of on-road assessment. Am J Occup Ther. 2010 Jan-Feb;64(1):114-22.
- DeGutis J. M., Van Vleet T. M. Tonic and phasic alertness training: a novel behavioral therapy to improve spatial and non-spatial attention in patients with hemispatial neglect. Front. Hum. Neurosci. 2010.Aug 24;4. pii: 60
- Van Vleet TM, Degutis JM. Cross-training in hemispatial neglect: auditory sustained attention training ameliorates visual attention deficits. Cortex 2013. 49, 679–690.
- Mazer BL, Sofer S et al. Use of the UFOV to evaluate and retrain visual attention skills in clients with stroke: a pilot study. Am J Occup Ther. 2001 Sep-Oct;55(5):552-7.
- Vance DE, Fazeli PL et al. Speed of Processing Training With Middle-Age and Older Adults With HIV: A Pilot Study. JANAC 2012; 23 (6); 500-10
- Kaur J, Dodson JE et al. Predictors of Improvement Following Speed of Processing Training in Middle-Aged and Older Adults With HIV: A Pilot Study. Journal of Neuroscience Nursing. 2014 Feb 46(1):23-33
- Rosen AC, Sugiura L et al. Cognitive Training Changes Hippocampal Function in Mild Cognitive Impairment: A Pilot Study. Jour of Alz Dis, Vol 26, Supp 3/2011, 349-357.
- Barnes DE, Yaffe K et al. Computer-based cognitive training for mild cognitive impairment: results from a pilot randomized, controlled trial. Alzheimer Dis Assoc Disord 2009 Sep;23(3):205-210.
- Edwards JD, Hauser RA et al. Randomized trial of cognitive speed of processing training in Parkinson disease. Neurology 2013 81(15):1284.
- Classen S, McCarthy DP et al. Useful Field of View as a Reliable Screening Measure of Driving Performance in People With Parkinson's Disease: Results of a Pilot Study. Traffic Injury Prevention 2009 10(6) 593-98.
- Badenes D, Garolera M et al. Driving competencies and neuropsychological factors associated to driving counseling in multiple sclerosis. J Int Neuropsychol Soc 2014 May 20(5): 555-65.
- Shawaryn MA, Schultheis MT et al. J. Assessing Functional Status: Exploring the Relationship Between the Multiple Sclerosis Functional Composite and Driving. Arch Phys Med Rehabil 2002;83:1123-9.
- Schultheis MT, Garay E, DeLuca J. The influence of cognitive impairment on driving performance in multiple sclerosis. Neurology 2001;56:1089–94
P1. Grimm G, Gill S, Saini G, Relova R, Hoblyn J, Lee T, Stasio C, Mahncke H, Dragg L. Web-based cognitive training in veterans with Bi-polar Disorder: A pilot study. Archives of Clinical Neuropsychology 2013, 28(6) B-33.
P2. Lebowitz M, Cantor J, Gordon W, Spielman L, Ashman T, Tsaousides T, Spina L. Examining the usability of a computerized cognitive training program in people with traumatic brain injury: a pilot study. Archives of Physical Medicine and Rehabilitation 2009;90:e18–e19.
P3. Voelbel, Ceceli A et al. C-40 Computerized Neuroplasticity Training Increases Processing Speed of Verbal Information: A Pilot Study of Adults with Traumatic Brain Injury. Arch Clin Neuropsychol. 2014 Sep;29(6):589.
P4. Kim SJ, Stasio C, Spina LM, Tinker DE, Mahncke HW. Enhanced Quality of Life in Individuals with “Chemobrain” After Using a Brain-Plasticity- Based Training Program. Psycho-Oncology 2008;17:S96
P5. Charvet L, Amelia M et al. Plasticity-Based Cognitive Remediation in Multiple Sclerosis (MS). Neurology 2014 Apr vol. 82 (10 Suppl) p3.134






 English
English
 Français
Français